Triple Negative Breast Cancer
Triple Negative Breast Cancer
What is a Triple Negative Breast Cancer?
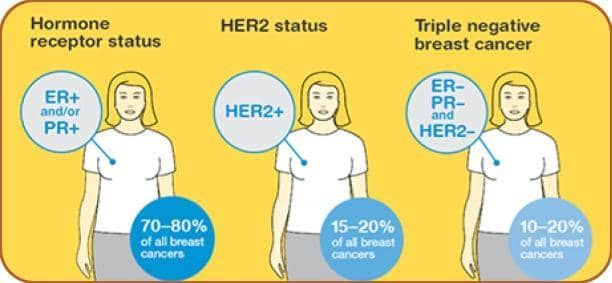
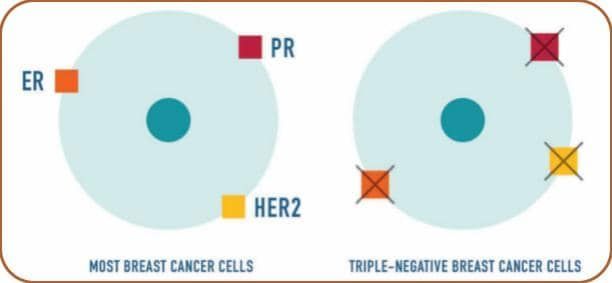
Triple Negative Breast Cancer, abbreviated to TNBC, is a unique subtype of breast cancer characterised by the absence of these three receptors (hence Triple Negative) on the cancer cells.
Breast cancer is not a singular entity. There are so many variables, and while most breast cancers fit into a particular mould, a smaller percentage are distinct and different. Understanding the characteristics and differences of t between triple-negative breast cancer and other types of breast cancer is crucial for accurate diagnosis and treatment planning.
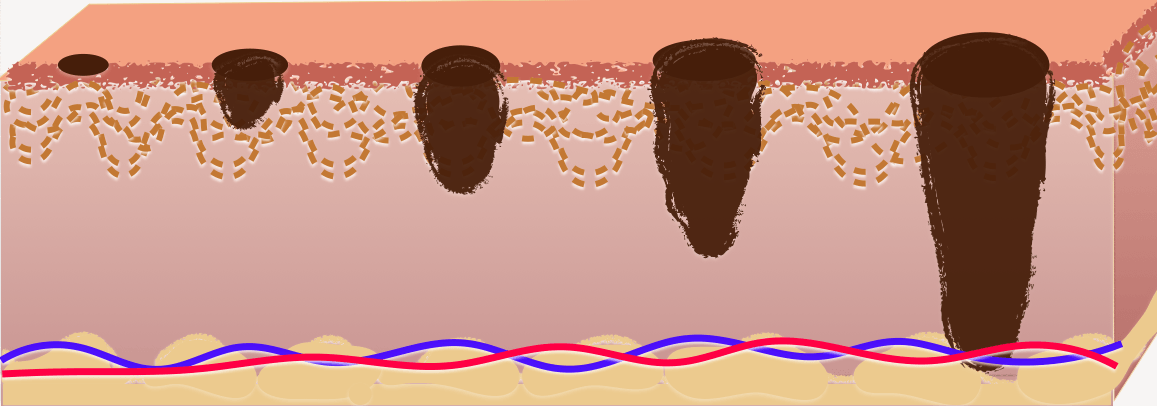
We determine the specific type of breast cancer based on the presence or absence of receptors, proteins found inside or on the surface of cells that trigger cellular responses. These receptors include the
- Oestrogen receptor (ER)
- Progesterone Receptor (PR)
- Human Epidermal Growth Factor Receptor 2 (HER2)
What is the Implication of Triple Negative Breast Cancer?
Treatment for breast cancers that are Oestrogen receptor-positive, Progesterone receptor-positive, or HER2-positive involves medications that target these receptors to prevent or slow cancer growth.
However, triple-negative breast cancers (TNBC) have no presence of these receptors, making traditional hormone and targeted therapies like Aromatase inhibitors, Tamoxifen and HER2-targeted therapies like Trastuzumab ineffective. Instead, chemotherapy has demonstrated greater efficacy in treating TNBC.
What is a Basal-Like Subtype?
Most TNBC cancers have a genetic pattern known as basal-like, meaning the cancer cells resemble the basal cells that line the breast ducts. Some may refer to triple-negative breast cancer as a basal tumour, basal breast cancer, or basal-like disease. Basal-like breast cancers tend to overexpress certain genes that promote cancer growth. Nevertheless, not all triple-negative breast cancers are basal-like, and not all basal-like breast cancers are triple-negative. Approximately 70 to 90 per cent of triple-negative breast cancers fall into the basal-like category.
What are the Broad Distinctions of Breast Cancer Types?
Some who have experienced breast cancer might not understand the differences between triple-negative breast cancers and hormone receptor-positive or HER2-positive breast cancers.
Others might be familiar with hormonal treatment pills that reduce the risk of recurrence, which may not apply to those with TNBC. Explaining these differences can be challenging, especially for those recently diagnosed. It is important to remember that some chemotherapy medicines used for other breast cancer types may also be employed for TNBC.
There are several myths surrounding TNBC, such as assuming that the same treatments used for other types of breast cancer will work exactly the same for TNBC or believing that TNBC is always challenging to treat. While TNBC can be aggressive, the effectiveness of treatment depends on various factors, including tumour size, lymph node involvement, other cancer factors and overall health.
Who Tends To Develop Triple-Negative Breast Cancer?
Age, Race, or Ethnicity
Several studies indicate that being premenopausal or having African ancestry increases the risk of developing basal-like or triple-negative breast cancer. Among African-American women with breast cancer, there is an estimated 20 to 40 per cent chance of triple-negative cancer. The reasons for the higher rates of triple-negative breast cancer in premenopausal women and specific ethnic groups are not yet fully understood.
Breast Cancer Gene Mutations
BRCA1 and BRCA2 genes are inherited from parents and when intact, typically function to prevent the development of cancers. However, only a small percentage of individuals with breast cancer have mutations in BRCA1 or BRCA2, which alter their DNA. Being born with a BRCA1 mutation increases the risk of developing basal-like breast cancer, though not all breast cancers resulting from BRCA mutations are triple-negative. BRCA2 mutations are more commonly associated with Oestrogen receptor-positive breast cancer.
Are Triple-negative breast cancers always difficult to treat?
While many triple-negative cancers are aggressive, the effectiveness of treatment depends on factors such as tumour size and lymph node involvement, in addition to its triple-negative status. Highly effective treatments, Chemotherapy and Immunotherapy are available for triple-negative breast cancer, and doctors work closely with patients to identify the most suitable approach.
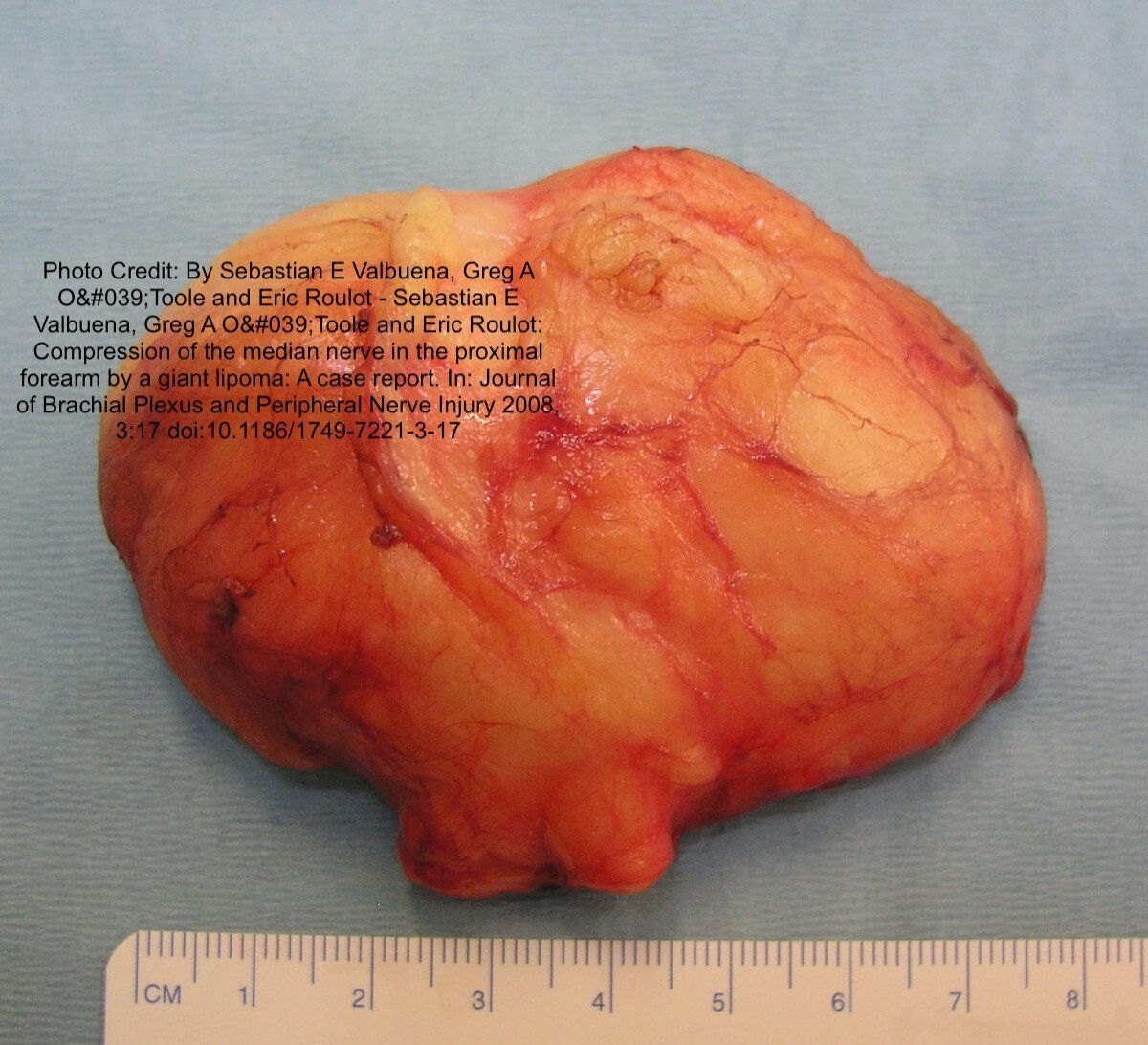
What is a Metaplastic Triple-Negative Breast Cancer?
This is a rare and aggressive subtype, less than 5% of all breast cancers, which accounts for only a small percentage of all breast cancer cases but poses unique challenges in diagnosis, treatment, and prognosis. Like invasive ductal cancer, metaplastic breast cancer begins in the breast's milk duct before spreading to the tissue around the duct. What makes it different is the kinds of cells that make up the cancer. When the cells are examined under a microscope, they may contain some abnormal-looking ductal breast cells, but they also contain cells that look like other tissues of the breast; for example, soft tissue and connective tissue in the breast. It appears that the ductal cells have changed form (metaplasia) to become completely different cells, though it is not known exactly how or why this occurs. Metaplasia refers to a process where cancer cells transform, taking on characteristics of different cell types from the surrounding tissues, making it challenging to classify and diagnose.
Metaplastic TNBC is a rare variant of triple-negative breast cancer, where the cancer cells not only lack the expression of Oestrogen receptors (ER), Progesterone Receptors (PR), and Human epidermal growth factor receptor 2 (HER2) but also exhibit metaplastic features. How to diagnose Metaplastic Triple-Negative Breast Cancer?
- Diagnosing metaplastic TNBC. This requires both histological and immunohistochemical analyses. An experienced pathologist looks for histological features in the biopsy specimen, such as squamous or spindle cell differentiation. Immunohistochemistry confirms the absence of ER, PR, and HER2 in the cancer cells.
- Clinical Characteristics and Prognosis. Metaplastic TNBC is known for aggressive behaviour, fast growth, and increased local and distant recurrence tendencies. It is associated with a poorer prognosis and overall survival rates compared to the more common breast cancer subtypes.
What Are The Treatment Options For Metaplastic TNBC?
Standard treatment options as for other triple-negative breast cancers. Targeted therapies like hormonal therapies and anti-HER2 agents are not useful. Neoadjuvant chemotherapy is often used to reduce cancer size before surgery, but the response to treatment may be variable. We also use immunotherapies and targeted agents for better treatment strategies. Recent studies have identified potential genomic and molecular alterations that could play a role in the development and progression of this subtype. This might help develop personalised therapies and improve treatment outcomes.
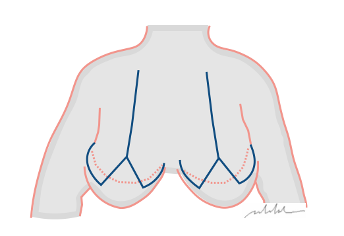
What Advancements In Surgical Techniques For Managing Triple Negative Breast Cancer?
Due to the lack of targeted therapies, surgery remains an essential component of the treatment approach. There have been significant advancements in surgical techniques to improve outcomes and preserve the quality of life for patients with this aggressive breast cancer subtype.
- Neoadjuvant Therapy and Surgery:
Chemotherapy or targeted therapy is utilised before surgery, shrinking cancer before surgery and potentially increasing the rate of breast-conserving surgery (lumpectomy) rather than mastectomy. It also for a better assessment of treatment response, helping us make more informed decisions on the most appropriate surgical strategy for each patient.
- Breast-Conserving Surgery (Lumpectomy) involves removing the tumour along with a margin of surrounding normal tissue. Advances in oncoplastic surgery have enabled us to combine oncological principles with plastic surgical techniques. And we get improved cosmetic outcomes while ensuring complete cancer removal, preserving the patient's breast appearance, body image and self-esteem.
- Sentinel Lymph Node Biopsy (SLNB) and Targeted Axillary Dissection(TAD) These are minimally invasive techniques that involve identifying and removing a few lymph nodes, which reduces the need for complete axillary lymph node dissection (ALND), reducing complications such as lymphoedema and improving patient recovery.
- Nipple-Sparing Mastectomy (NSM):
When prophylactic or therapeutic mastectomy is needed, nipple-sparing mastectomy can be performed without removing the nipple-areola complex, resulting in a more natural breast appearance and improved body image. This technique offers excellent aesthetic outcomes and improved psychological well-being.
Advancements in surgical techniques have significantly transformed the management of triple-negative breast cancer, offering improved treatment outcomes and enhanced quality of life for patients.
Neoadjuvant therapy, oncoplastic surgery, and intraoperative technologies have radically changed the surgical landscape, providing individual solutions to each patient's needs. Surgeons and multidisciplinary teams constantly refine these techniques, creating a way for more personalised and excellent surgical approaches for patients with triple-negative breast cancer.
References:
- Lehmann BD, Bauer JA, Chen X, et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest. 2011 Jul;121(7):2750-67. doi: 10.1172/JCI45014.
- Sharma P. Biology and management of patients with triple-negative breast cancer. Oncologist. 2016 Jan;21(1):105-17. doi: 10.1634/theoncologist.2015-0338.
- Anders CK, Carey LA. Biology, metastatic patterns, and treatment of patients with triple-negative breast cancer. Clin Breast Cancer. 2009 Dec;9 Suppl 2:S73-81. doi: 10.3816/CBC.2009.s.008.
- Pareja F, Geyer FC, Marchiò C, et al. Metastasis-Free Survival Is Associated With Overall Survival in Patients With Metaplastic Breast Cancer. NPJ Breast Cancer. 2020 Feb 14;6:7. doi: 10.1038/s41523-020-0143-5.
- Alvarado R, Yi M, Le-Petross H, et al. The role for sentinel lymph node dissection after neoadjuvant chemotherapy in patients who present with node-positive breast cancer. Ann Surg Oncol. 2012 Mar;19(3):317-21. doi: 10.1245/s10434-011-2025-y.
- Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomised study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002 Oct 17;347(16):1227-32. doi: 10.1056/NEJMoa020989.
Social Listings