Gynaecomastia
Gynaecomastia
What is Gynaecomastia?
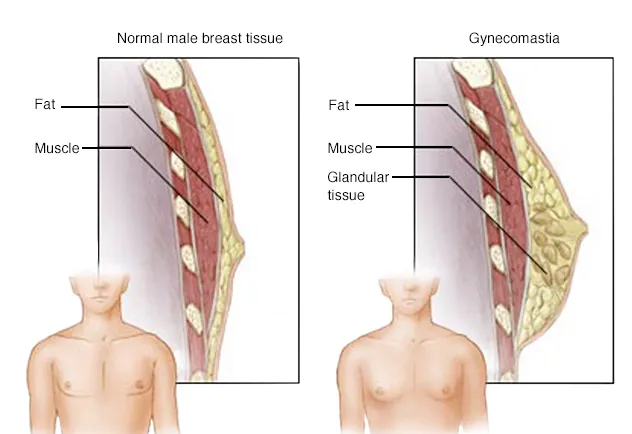
Gynaecomastia is an increase in the amount of breast gland tissue in boys or men, caused by an imbalance of the hormones oestrogen and testosterone. It can affect one or both breasts, sometimes unevenly. Pseudogynaecomastia refers to an increase in fat but not glandular tissue in male breasts. Newborns, boys going through puberty and older men may develop gynaecomastia as a result of normal changes in hormone levels, though other causes also exist.
Usually, gynaecomastia is not a serious problem, but it can be difficult to cope with the condition. Men and boys with may have pain in their breasts and may feel embarrassed. It may go away on its own, however if persists, medication or surgery may be needed.
What are the symptoms of gynaecomastia?
Most adult men have no symptoms. Signs and symptoms of the condition may include:
- Pain, particularly in adolescents
- Swollen breast tissue
- Breast tenderness
- Nipple sensitivity with rubbing against clothes
When to see a doctor for gynaecomastia?
See your doctor if you have:
- Swelling
- Pain or tenderness
- Nipple discharge in one or both breasts
What causes gynaecomastia?
It is triggered by a decrease in the amount of the hormone testosterone compared with Oestrogen. The decrease can be caused by conditions that block the effects of testosterone, reduce testosterone or increase Oestrogen level. Several things can upset the hormone balance, including the following.
What are natural hormone changes in the body during puberty?
The hormones testosterone and oestrogen control sex characteristics in both men and women. Testosterone controls male traits, such as muscle mass and body hair. Oestrogen controls female traits, including the growth of breasts.
Most people think of oestrogen as an exclusively female hormone, but men also produce it, usually in small quantities. Male oestrogen levels that are too high or are out of balance with testosterone levels can cause gynaecomastia.
- Gynaecomastia in infants. More than half of male infants are born with enlarged breasts due to the effects of their mother's oestrogen. Generally, the swollen breast tissue goes away within two to three weeks after birth.
- Gynaecomastia during puberty. Gynaecomastia caused by hormone changes during puberty is relatively common. In most cases, the swollen breast tissue will go away without treatment within six months to two years.
- Gynaecomastia in adults. Researchers have estimated that the prevalence among men ages 50 to 80 is between 24% and 65%.
However, most men with the condition experience no symptoms.
What are medications or substances that can cause gynaecomastia?
A number of medications which include:
- Anti-androgens used to treat an enlarged prostate, prostate cancer and other conditions. Examples include flutamide, finasteride and spironolactone.
- Anabolic steroids and androgens to treat hormone deficiencies, delayed puberty, or muscle loss from another disease.
- AIDS medications. The oestrogen-like properties of some HIV medications can cause gynaecomastia.
- ADHD medications that contain amphetamines.
- Anti-anxiety medications, such as diazepam.
- Tricyclic antidepressants.
- Antibiotics.
- Ulcer medications, such as the over-the-counter drug cimetidine.
- Chemotherapy to treat cancer.
- Heart medications, such as digoxin and calcium channel blockers.
- Stomach-emptying medications, such as metoclopramide.
Recreational drugs, illicit drugs and alcohol
Substances that can cause gynaecomastia include:
- Alcohol
- Anabolic steroids used to build muscle and enhance athletic performance
- Amphetamines
- Marijuana
- Heroin
- Methadone
What are health conditions that can cause gynaecomastia?
Several health conditions can cause gynaecomastia by affecting the balance of hormones. These include:
- Hypogonadism. Conditions that lower testosterone production, such as Klinefelter syndrome or pituitary insufficiency, can be associated with gynaecomastia.
- Aging. Hormone changes that occur with aging can cause it, especially in men who are overweight.
- Tumours. Some tumours, such as those involving the testes, adrenal glands or pituitary gland, can produce hormones that alter the male-female hormone balance.
- Hyperthyroidism. The thyroid gland produces too much of the hormone thyroxine.
- Kidney failure. Half the people being treated with dialysis experience it due to hormonal changes.
- Liver failure and cirrhosis. Changes in hormone levels related to liver problems and cirrhosis medications are associated with gynaecomastia.
- Malnutrition and starvation. When your body is deprived of adequate nutrition, testosterone levels drop while oestrogen levels remain the same, causing a hormonal imbalance. Gynaecomastia can also happen when normal nutrition resumes.
Herbal products
Plant oils, such as tea tree or lavender, used in shampoos, soaps or lotions have been associated with gynaecomastia. This is probably due to their weak oestrogenic activity.
What are risk factors for gynaecomastia?
Risk factors for gynaecomastia include:
- Adolescence
- Older age
- Use of anabolic steroids to enhance athletic performance
- Certain health conditions, including liver and kidney disease, thyroid disease, hormonally active tumours, and Klinefelter syndrome
What are complications of gynaecomastia?
Gynaecomastia has few physical complications, but it can cause psychological or emotional problems caused by appearance.
How can gynaecomastia be prevented?
There are a few factors you can control that may reduce the risk of gynaecomastia:
- Don't use drugs. Examples include anabolic steroids, amphetamines, heroin and marijuana.
- Avoid alcohol. Don't drink alcohol. If you do drink, do so in moderation.
What tests can be done for gynaecomastia?
Your doctor will likely order tests to identify a possible cause of gynaecomastia, to screen for possible breast cancer and to rule out other conditions. These may include:
- Blood tests
- Mammograms
- Computerized tomography (CT) scans
- Magnetic resonance imaging (MRI) scans
- Testicular ultrasounds
- Tissue biopsies
What conditions can cause similar symptoms like gynaecomastia?
Your doctor will want to be sure that your breast swelling is gynaecomastia and not another condition. Other conditions that can cause similar symptoms include:
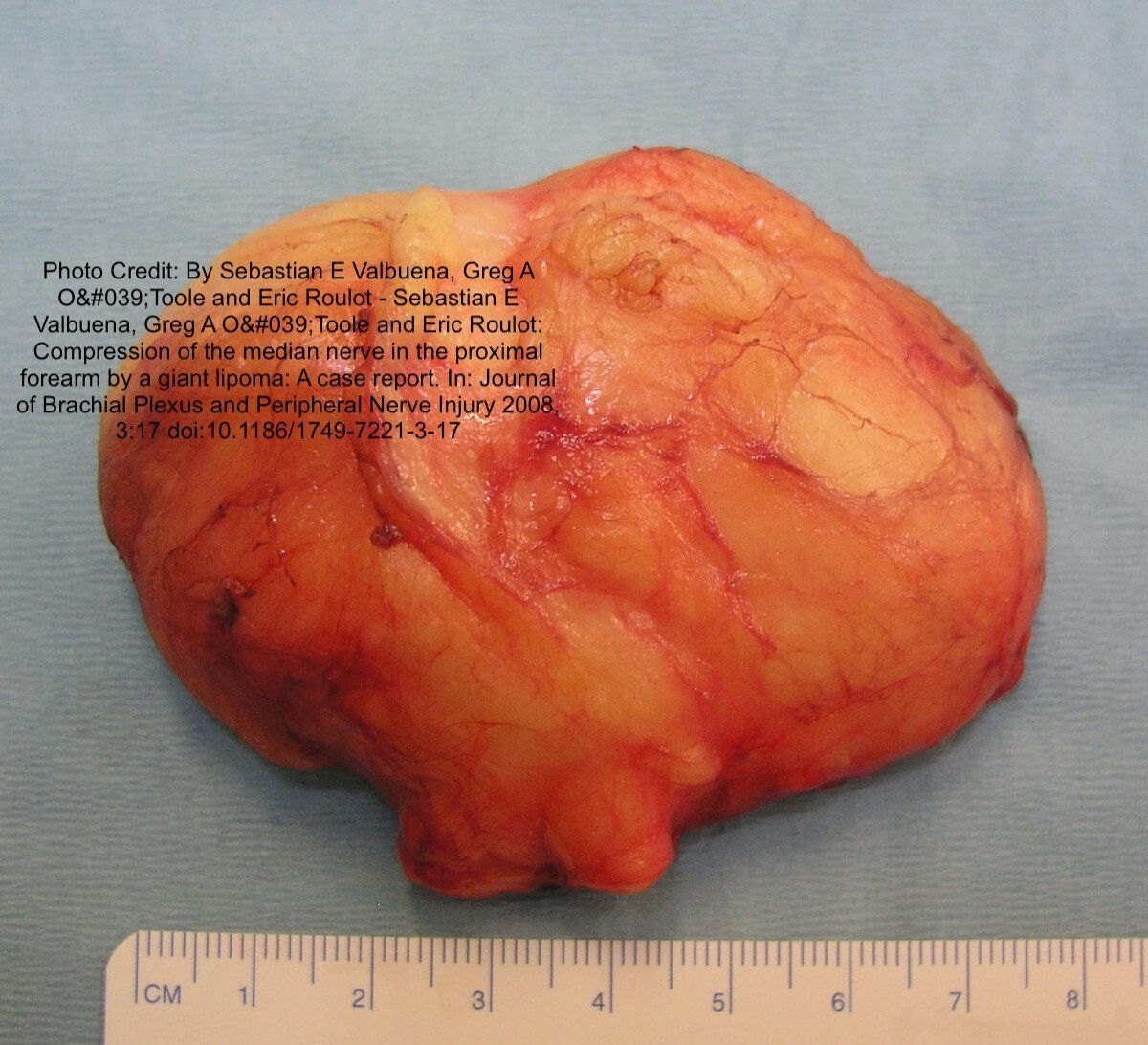
- Fatty breast tissue (pseudogynaecomastia). Some men and boys, especially those with obesity, have breast fat that resembles gynaecomastia. This isn't the same as gynaecomastia and doesn't need additional evaluation.
- Breast cancer. Breast cancer is uncommon in men but can occur. Enlargement of one breast or the presence of a firm nodule raises the concern for male breast cancer.
- A breast abscess. This is an infection of the breast tissue.
What is the treatment for gynaecomastia?
Most cases of gynaecomastia resolve over time without treatment. However, if gynaecomastia is caused by an underlying condition — such as hypogonadism, malnutrition or cirrhosis — that underlying condition may need treatment.
If you're taking medications that may be the cause of gynaecomastia, your doctor may recommend stopping them or substituting another medication.
In adolescents with no apparent cause of gynaecomastia other than normal hormone changes during puberty, the doctor may recommend periodic reevaluations every three to six months to see if the condition improves on its own. Gynaecomastia in adolescents often goes away without treatment in less than two years.
Treatment may be necessary if gynaecomastia doesn't improve on its own or if it causes significant pain, tenderness or embarrassment.
What medications can be used to treat gynaecomastia?
Medications used to treat breast cancer and other conditions may be helpful for some men with gynaecomastia. They include:
- Tamoxifen
- Aromatase inhibitors, such as anastrozole
Although these medications are approved by the Food and Drug Administration, they have not been approved specifically for use in people with gynaecomastia.
What is the role of surgery to remove excess breast tissue in gynaecomastia?
If enlarged breasts are significant and bothersome even after initial treatment or observation, your doctor may advise surgery.
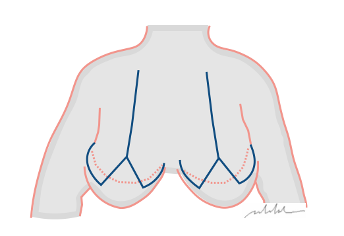
Two gynaecomastia surgery options are:
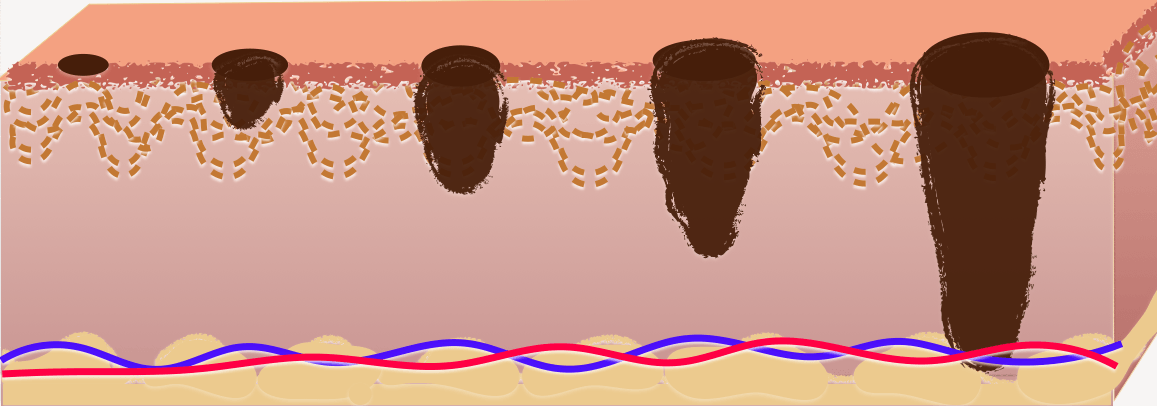
- Liposuction. This surgery removes breast fat but not the breast gland tissue itself.
- Mastectomy. This type of surgery removes the breast gland tissue. The surgery is often done using only small incisions. This less invasive type of surgery involves less recovery time.
What are measures for coping and support for patients with gynaecomastia?
For men, enlarged breasts can be stressful and embarrassing. Gynaecomastia can be difficult to hide and a challenge to romantic relationships. During puberty, gynaecomastia can make boys a target for teasing from peers. It can make activities such as swimming or changing in the locker room traumatic.
Whatever your age, you may feel like your body has betrayed you and you may feel unhappy with yourself. These feelings are normal, but to help you cope you can:
- Get counseling. Talk therapy can help you avoid anxiety and depression caused by gynaecomastia. It can also help you communicate with your partner or family members so that they understand what you're going through.
- Reach out to your family and friends. You may feel embarrassed to talk about gynaecomastia with the people you care about. But explaining your situation and asking for support will likely strengthen your relationships and reduce stress.
- Connect with others who have gynaecomastia. Talking with men who have had a similar experience can help you cope.
Social Listings