THERAPEUTIC MAMMOPLASTY
WHAT IS A THERAPEUTIC MAMMOPLASTY?
Therapeutic mammoplasty is a work of art. It is essentially surgery to remove breast cancer (therapeutic) and then reshape the breast by removing skin and breast tissue (mammoplasty). The aim is to try to preserve a normal breast shape that will usually be smaller and more uplifted. There is a limit to how much breast tissue can be removed with a standard lumpectomy without adversely affecting the appearance of the breast, but this technique allows us to remove more breast tissue and attempt to leave an acceptable cosmetic outcome.
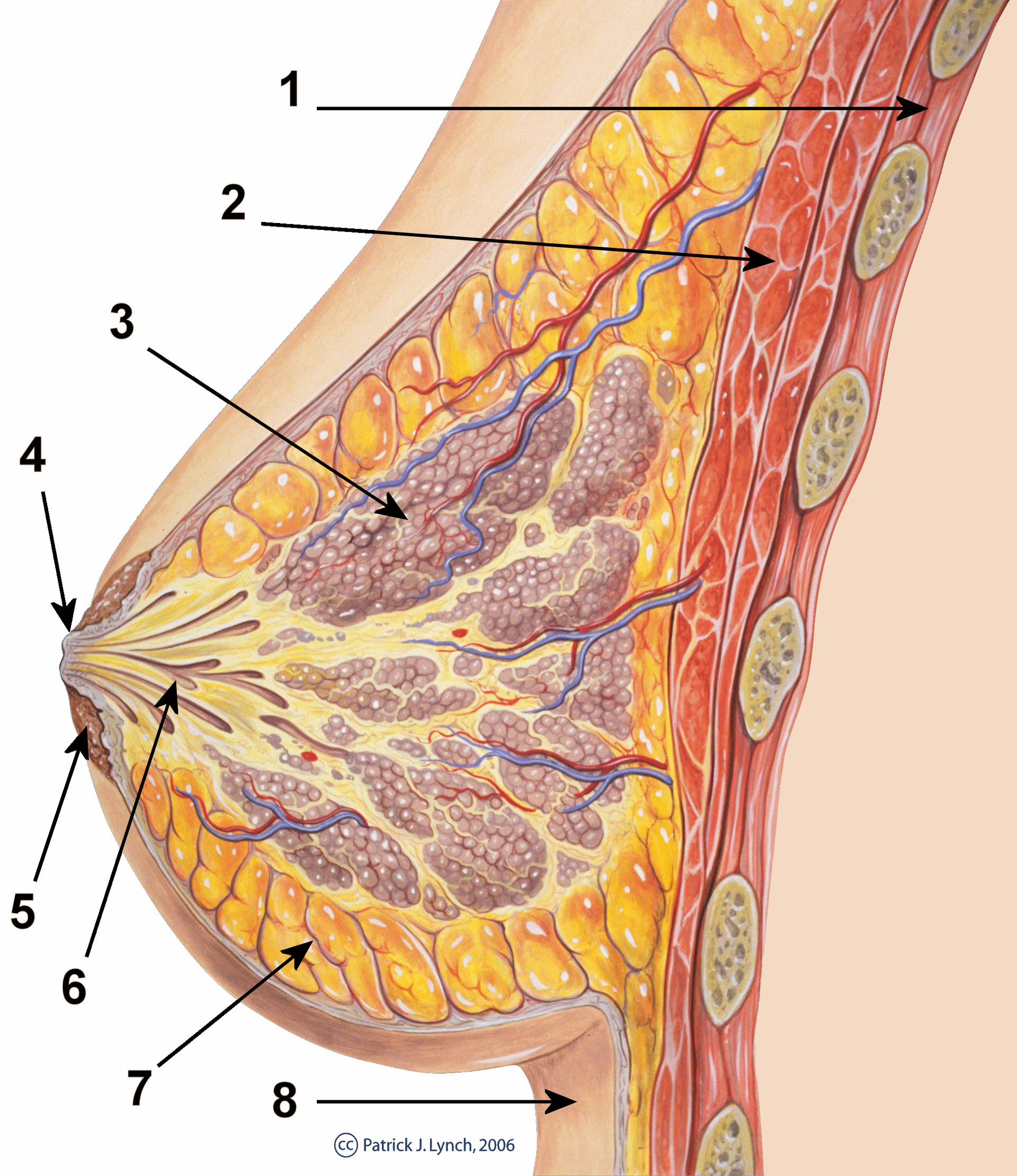
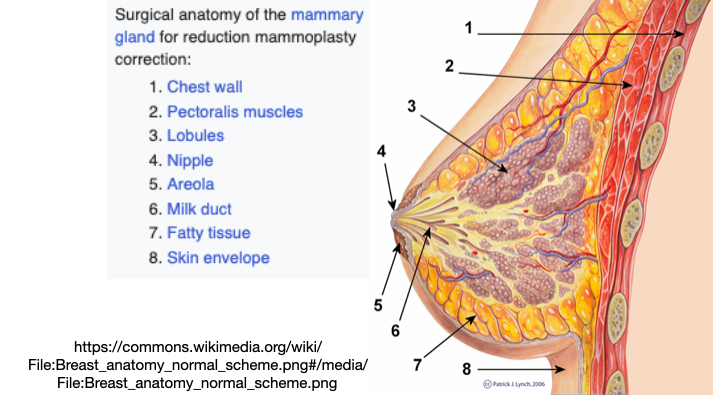
The operation is suitable for women with moderate to larger breasts, and who have a degree of droop (ptosis). If there is significant asymmetry (difference between your breasts), the breast on the other side may also need to be reduced, to provide a better match in size and shape if so desired. This is known as symmetrisation surgery and ideally is done at the same time, however can be performed at a later date if preferred. Picture below shows the anatomy of the breast, 'mammary gland.'
WHAT ARE THE ADVANTAGES?
The technique aims to produce a normal breast shape with no indentation, distortion or loss of cleavage that might otherwise be likely. It is particularly useful for lower breast tumours that are more likely to develop a deformity if a simple lumpectomy,
Breast Conserving Surgery is performed.
For women with larger breasts, with back pain, neck pain and heaviness who desire smaller breasts this is an added benefit.
For women with very large breasts, reducing the size makes radiotherapy more conducive.
What are the disadvantages?
The surgery is more extensive than a simple lumpectomy with longer albeit well hidden wounds.
There are more risks associated with the surgery, including altered nipple sensation or numbness, potential for nipple necrosis (1%), and fat necrosis, and problems with wound healing.
A specific cosmetic outcome cannot be guaranteed and there is still a risk you may have a degree of distortion or indentation.
There might be a need for re operation should we not get clear surgical margins around the area of disease; oncological safety is always the primary goal.
Is there an alternative?
The other surgical options are to have a simple lumpectomy (wide local excision) without reshaping the breast, or to have a mastectomy and remove all of the breast tissue; this can be done with immediate or delayed reconstruction.
What does the operation involve?
On the morning of surgery your surgeon will do some marking on you to plan out the operation and may take some photographs. You will also meet the anaesthetist. If the tumour is difficult to feel, you may need to go to the X-ray Department before the surgery for the Radiologist to localise the tumour/or a previously inserted clip and put a
hookwire (guide) into it under local anaesthetic, as a guide to which breast tissue to remove.
The operation may also involve surgery to your lymph glands in your armpit,
Sentinel Node Biopsy. This is done to assess whether the cancer has spread to any of the lymph nodes (also called glands) as this information helps plan any further treatment you may need. This procedure requires a preoperative test called a ‘Lymphoscintigram’.
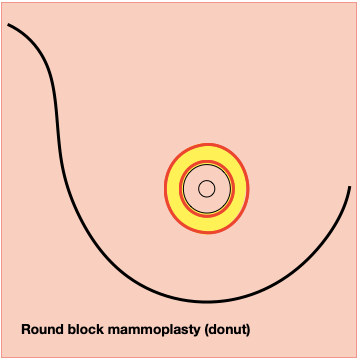
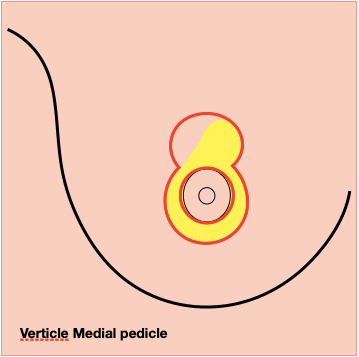
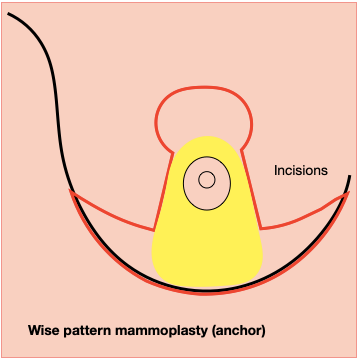
To perform the operation, the tumour and a margin of tissue around it are removed first, and then the breast is reshaped with the nipple repositioned. The full extent of surgery depends on the technique being used:
Occasionally it may be necessary to remove the nipple if the breast cancer lies close to the centre of the breast. If removal of the nipple is required, a new nipple can be reconstructed at a later date, usually under local anaesthetic.
At the same time, some or all of the lymph nodes may be removed from the armpit. This is done to assess whether the cancer has spread to any of the lymph nodes (also called glands) as this information helps plan any further treatment you may need.
This procedure usually results in a significant breast lift, reduced volume and major shape change. Most patients usually decide to have surgery to the other breast at the same operation to create better symmetry.
Are there any complications for this surgery?
All surgery carries some element of risk. The breast may be painful, swollen and bruised following your operation. Most complications can be detected and treated without difficulty, some need further surgery, like
Lipofilling for further reshaping, Scar revision, Reexcision.
General complications
- Haematoma: This is bleeding into the tissues following surgery and can occasionally lead to patients returning to theatre to stop the bleeding and remove the blood (3-4 in every 100 women).
- Wound infection: This can occur after any type of surgery and may need treatment with antibiotics.
- Deep venous thrombosis/pulmonary embolism: This can happen after any operation and general anaesthetic. Risks are reduced by wearing preventative stockings and giving an anti- clotting injection in certain cases.
Specific complications
- Re-excision (need for further surgery): If we are unable to get a clear margin of normal tissue around the lump then usually further surgery will be required on your breast (20% - 2 in 10 cases). We will not know this until you attend for your results between 3-4 weeks later. If this is needed it can sometimes be done through the same incision, as a day case and performed within 4 weeks, but other times a mastectomy may be advised.
- Delayed wound healing: The blood supply at the point where the vertical scar meets the horizontal scar (the T-junction) is the poorest and so this area is vulnerable. The skin may fail to heal and will separate leaving a raw area, and is occasionally extensive, requiring regular dressings for several months until the wound is fully healed. Delayed healing can occur in 3 – 5% (between 3 and 5 cases out of every 100).
- Nipple complications: The operation by its nature partially disrupts the blood supply to the nipple. There is a small but definite risk of nipple loss from this type of surgery, either total or partial (less than 1% - 1 in 100 cases). The risk is greater the closer the tumour is to the nipple. Loss of, or altered, nipple sensation is a more common complication seen in 30-50% of patients; this may be a temporary or permanent symptom.
- Asymmetry: There may be some lasting differences in the size and shape of your breasts following surgery. As mentioned earlier, this may result in a significant difference. You may desire the breast on the other side to be reduced at the same time to provide a good match in size and shape.
- Scarring: Initially, the scars will be fine, bright red lines; in most cases the scars will usually heal satisfactorily and soften, becoming much paler and less obvious after 12 months or so. Some patients have a tendency to form red and lumpy scars (hypertrophy) or keloid scars, which are broad raised scars. The scarring will be permanent.
- Fat necrosis: This is a common complication with this type of surgery due to interruption to the delicate blood supply of the fatty tissue within the breast. Occasionally, this fat dissolves and turns into a yellow, oily fluid that can leak through the wound closure. It more commonly results in a lump or hard areas within the breast and may occur several months after surgery. Any breast lumps found should be checked with GP and/or mentioned at follow-up appointment.
What to expect after the operation
You will go back to the ward and we will encourage you to get up and move around. If you have a drain it is usually removed the following day and then you can go home.
You will need to take regular painkillers following surgery. You may experience some shooting pains in the breasts - these will ease over the next few months. The breasts will be swollen and your nipple sensation may be altered. The swelling and bruising subside in 4-6 weeks but can take 6-12 months for the scars and shape of the breasts to settle.
Wound care
Your wound will be covered with a waterproof dressing to keep it clean. You are able to shower the day following surgery. There will be swelling and some discharge from the wound when you are at home, this may produce some blood staining on your bed clothes or bed sheets. This is nothing to worry about. Please contact your breast care nurse for advice or attend our clinic if you have concerns. Stitches are dissolvable.
If you feel unwell with a temperature, vomiting or notice significant redness of the skin on or around the breasts you should either contact your GP or Emergency department, if out of normal working hours, as you may have an infection and will need antibiotics. Sometimes fat necrosis is mistaken for infection, with redness and swelling but you are not unwell and there is no significant wound discharge.
Bras and prosthesis
You should wear a soft supportive bra (no underwiring) immediately after the operation. This helps prevent the weight of the breasts pulling on the wounds and affecting the healing process. You should wear the supportive bra for four to six weeks day and night, only taking it off to shower.
If there is a significant difference in size it may be necessary to wear a partial prosthesis in your bra, this can be discussed with your breast care nurse who will advise you about fitting.
Time off work
The length of time you need to take off work depends on the nature of your job but plan for two to four weeks. Please ask staff if you require a medical certificate and this will be given to you before you leave hospital.
Resuming normal activities
You are advised to avoid strenuous exercise for a minimum of six weeks. You are advised not to have sex for at least a week following the surgery as sexual arousal can cause further swelling of the breasts. Allow only gentle contact with your breasts for about six weeks.
You are advised not to drive for up to two weeks following surgery and only when you can safely perform an emergency stop.
Avoid heavy lifting, including vacuuming, washing and carrying heavy shopping.
Do not undertake exercises for 10 days following surgery. If you have ongoing problems with shoulder or arm stiffness, we will refer you to the physiotherapist.
Follow up treatment
You will be seen our clinic 7-14 days after your surgery to review the results of the surgery and remove your dressings. It may be helpful to bring a relative or friend with you to discuss the results and additional treatment you may require.